SOAP Note
What does "SOAP Note" mean in a report or doctor's letter? In our medical dictionary, you will find a patient-friendly explanation of the meaning of this medical term.
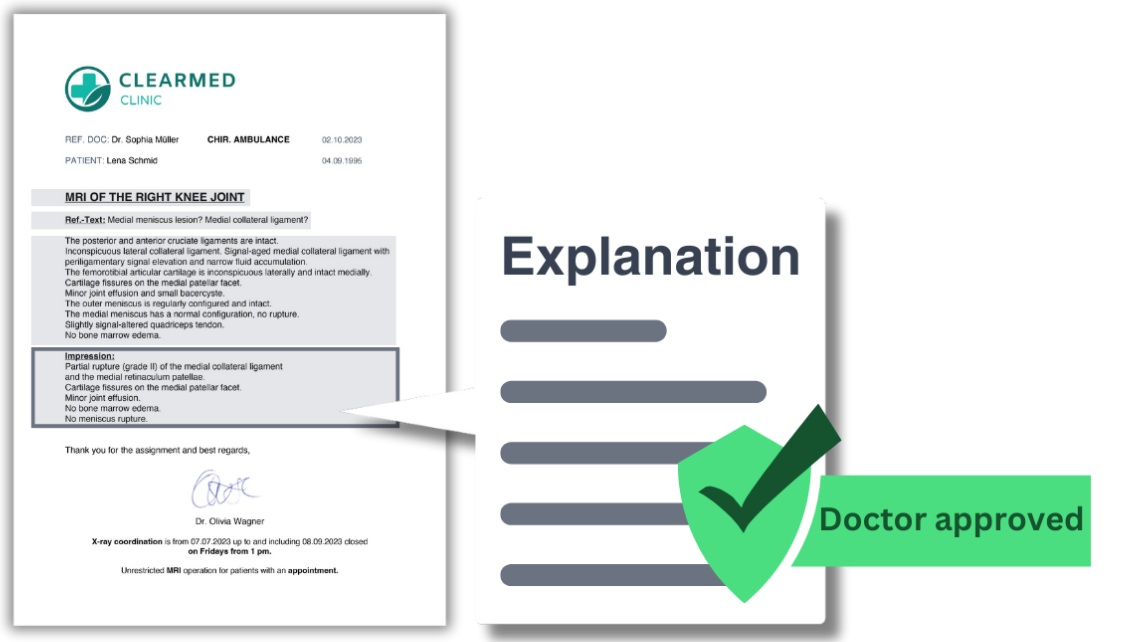
Explanation
A SOAP Note is a method used by healthcare professionals to document a patient's condition and treatment. The acronym stands for Subjective, Objective, Assessment, and Plan. "Subjective" refers to what the patient says about their condition, "Objective" is what the healthcare professional observes, "Assessment" is the professional's diagnosis based on the subjective and objective information, and "Plan" is the course of action for treating the patient. This method helps ensure clear and organized communication among healthcare professionals.

Confusing Medical Report?
BaluMed makes medicine understandable! Our extensive medical report explanation 'translates' complex medical terms from MRI findings and discharge summaries into easily understandable language. With a combination of artificial intelligence and medical expertise, we offer quickly available and reliable information.
- Extensive. Summary, explanation per section, glossary.
- Fast & Reliable. Doctor-reviewed, receive today.
- Privacy. Documents are automatically anonymized.
- Multilingual. English or German.
